The authors of a recent study1 have taken a novel look at the impact of venous thromboembolism (VTE) among hospitalized cancer patients in the US, finding that the risk of VTE increased significantly in hospitalized patients suffering from additional major medical comorbidities and that medical costs almost doubled in hospitalized cancer patients with VTE compared to those without it.
The study by Lyman et al. analysed nearly 6 million hospitalizations of 3,146,388 individual patients with cancer from more than 200 institutions in the US between 1995 and 2012. In evaluating the association of comorbidities on in-hospital mortality and medical costs of hospitalized cancer patients, the Seattle-based team of researchers found that the risk of VTE increased progressively from 2.3% in those with no comorbidities to over 11% for patients with 4 or more comorbidities – and that medical costs almost doubled in hospitalized cancer patients with VTE compared to those without it. Moreover, the risk of in-hospital mortality was exceptionally higher in cancer patients also suffering from additional major medical comorbidities, with the strongest risk factors caused by infectious complications such as sepsis (14%), invasive candidiasis (16%), pneumonia (11%) and IV line infections (14%).
VTE is a leading cause of morbidity and mortality among hospitalized patients with cancer, though much of the information on risk factors associated with VTE hospitalization in patients with cancer has come from studies involving seriously ill patients with small subgroups of patients with cancer. While current guideline recommendations call for thromboprophylaxis in most hospitalized patients with cancer, the risk of serious and life-threatening complications in such patients is greatest in those with major medical comorbidities and complications of cancer treatment.
Researchers evaluated VTE in hospitalized cancer patients, considering the presence of major comorbidities such as diabetes, and cerebrovascular, peripheral-vascular, heart, liver, lung, and renal disease. Study outcomes included VTE, in-hospital mortality and estimated cost of hospitalization.
According to the data, VTE was reported in 8.4% of patients when all admissions were considered during the time period. Figure 1 shows that the risk of in-patient mortality in patients with VTE was greater for the cohort suffering from multiple comorbidities and those with infection. VTE was diagnosed in 166,547 (5.3%) of individual patients, including 56,125 (1.8%) with pulmonary embolism (PE).
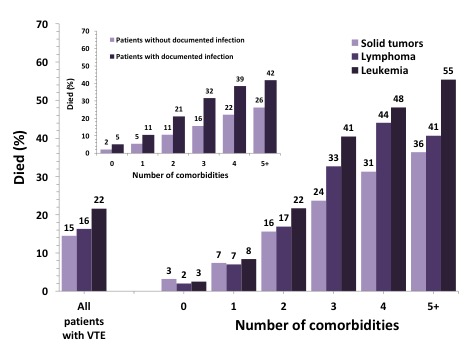
VTE was diagnosed in 5.2%, 5.8% and 5.4% of patients with solid tumors, lymphoma, and leukemia, respectively. Rates of VTE were greatest among patients with pancreatic (10.2%), gastric (7.1%) or other abdominal malignancies as well as those with ovarian (7.1%), lung (6.8%), and esophageal cancers (6.3%). The data collected showed that the reported rate of VTE had increased progressively from 3.5% in 1995 to over 6.5% in 2012 with the rate of PE increasing from 0.8% in 1995 to 2.3% in 2012. For hospitalized patients receiving cancer chemotherapy, the annual rate of VTE more than doubled from 3.6% in 1995 to 8.3% in 2012. During this same time period, imaging related to VTE decreased with significantly lower rates of CT, vascular ultrasound and ventilation perfusion lung scans reported. While reported rates of VTE increased, the length of hospital stay and in-hospital mortality decreased for those with as well as without VTE. The risk of VTE increased progressively from 2.3% in those with no comorbidities to over 11% for patients with 4 or more. The strongest risk factors for VTE were infectious complications including sepsis (14%), invasive candidiasis (16%), pneumonia (11%) and IV line infections (14%). In-hospital mortality was reported in 5.5% of cancer patients without VTE and in 15.0% of those with VTE including 19.4% of those with pulmonary embolism.
Regarding the rise in medical costs for such patients, average costs per hospitalization with and without VTE were $37,352 and $19,994 respectively, representing an increase of nearly 50% between 1995 and 2012.
References
Lyman GH, Culakova E, Poniewierski MS, Kuderer NM. Morbidity, Mortality and Costs Associated with Venous Thromboembolism in Hospitalized Patients with Cancer. https://doi.org/10.1016/j.thromres.2018.01.028
