Cancer is associated with an increased risk of venous but also arterial thrombosis1.
Moreover, contemporary anticancer therapy and supportive care allow for treatment of older patients with comorbid diseases such as ischemic heart disease and atrial fibrillation. The incidence, degree and duration of thrombocytopenia in cancer patients are variable2 and especially high in hematological malignancy. Regardless of the etiology, thrombocytopenia complicates antithrombotic therapy. Accordingly, antithrombotic therapy prescribed for a variety of indications in the context of thrombocytopenia is a common problem seen in up to 45% of cancer patients 4 and encountered by hematologists on a weekly basis3.
Management framework and guidelines
Management of antithrombotic therapy with concomitant thrombocytopenia is complex and informed mainly by expert opinion5, descriptive case series6 and retrospective studies on venous thromboembolism (VTE), as clinical trials of anticoagulants in VTE exclude patients with thrombocytopenia (<50-75×109/L)7-9. The first step of a management framework3 is as follows:
- continue or hold antithrombotic medication?; if continue,
- change medication type?; and/or
- reduce dose?; if hold,
- consider an inferior vena cava filter?
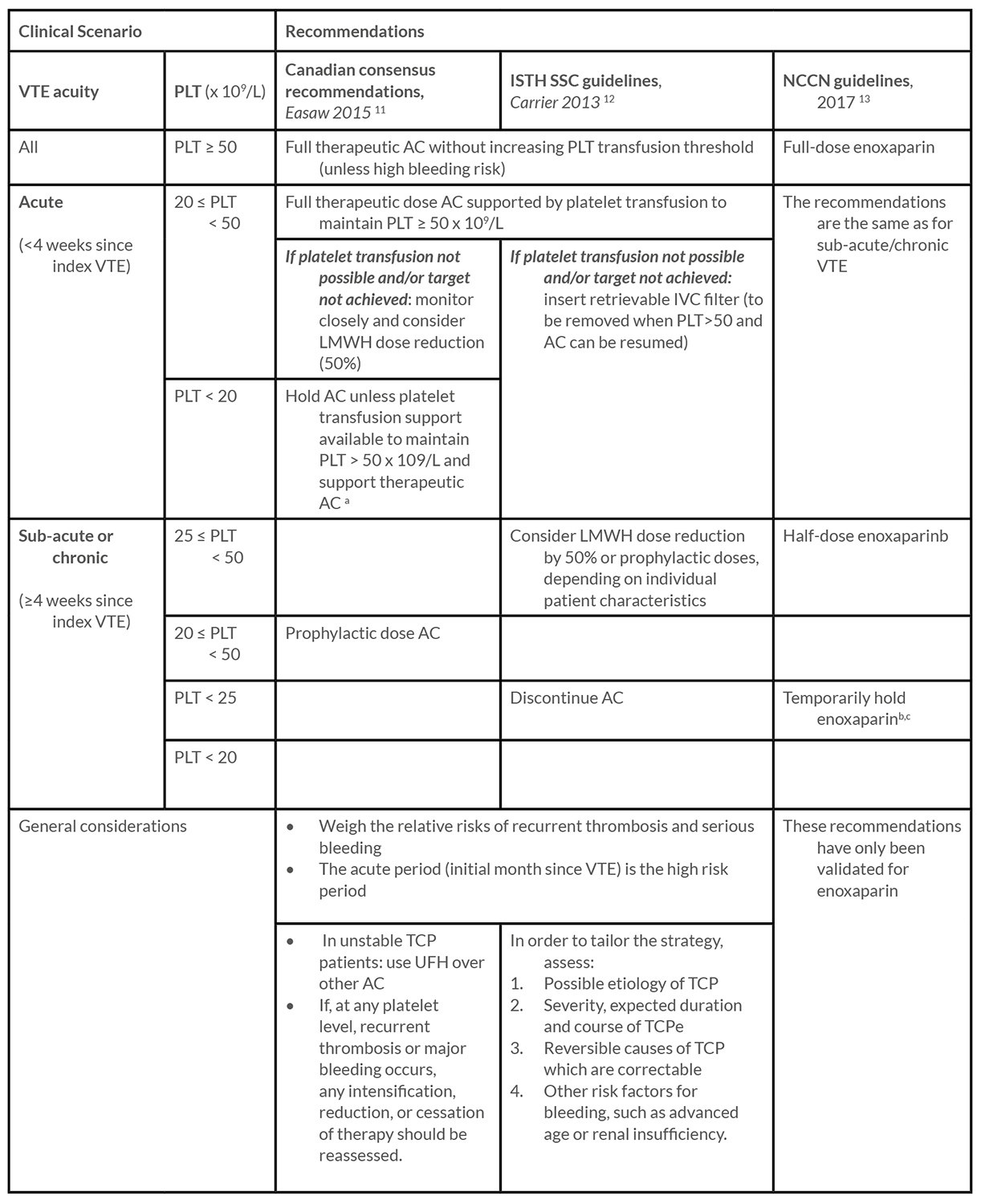
Next is deciding whether to increase the threshold for prophylactic platelet transfusion, above the standard 10×109/L10. Specific recommendations on management of thrombocytopenic patients with anticoagulation for VTE in cancer, but not other thrombocytopenic settings, are provided by 3 guidelines11-13, which use VTE acuity and platelet count to guide management, as summarized in Table 1.
This table includes the adapted recommendation statements from the guidelines, according to clinical scenarios. Additional considerations mentioned in these documents appear as footnotes or general considerations. a A temporary IVC filter in acute DVT can be considered on a case by case basis b This recommendation applies for both acute and non-acute VTE c If high risk of recurrent VTE and prolonged TCP is anticipated, consider increasing platelet transfusion threshold to 25 x 109/L to enable continuation of enoxaparin d If clinically significant VTE (i.e. severe symptoms, recurrence or progression on reduced or held doses of LMWH, hemodynamic instability) consider platelet transfusions as inpatient to maintain PLT > 50 x 109/L and support therapeutic AC until stable e for example: transient vs. permanent TCP; Is the current platelet count the nadir or it will drop further? AC, anticoagulation; DVT, deep vein thrombosis; ISTH SSC, international society on thrombosis and haemostasis, scientific standardization committee; IVC, inferior vena cava; LMWH, low molecular weight heparin; NCCN, national comprehensive cancer network; PLT, platelet count; TCP, thrombocytopenic; UFH, unfractionated heparin; VTE, venous thromboembolism
Emerging evidence
Additional insight is provided by recent small to moderately-sized retrospective cohort studies (N:47-204)14-19 in which anticoagulation was continued in 19%-79% of patients and held in 19%-63%14-19. Importantly, below the 50 x 109/L threshold, an influence of platelet counts on outcomes in anticoagulated patients remains unproven, while additional factors influence bleeding risk, underlining the complexity of this scenario23,36,37.
Finding the balance
The risk of recurrence is high with acute VTE (up to 47% at 90 days), even with full anticoagulation14,15,19, while some studies enriched with non-acute VTE show low recurrence rates (<1.5%)17,18. Holding appears to increase the risk of VTE recurrence, especially in acute VTE14,16. However, there is a high risk of clinically significant bleeding (13.5-27%)14-16,19 and a varying risk of major bleeding17,19, particularly when anticoagulation is continued. Taken together, the high rates of recurrent thrombosis alone suggest that anticoagulation should be administered during the acute period unless an absolute contraindication exists, in line with current guidelines11,12, whilst considering management approaches and patient selection strategies which may mitigate the bleeding risk. On the other hand, temporarily withholding anticoagulation during thrombocytopenia (<50 x 109/L) in patients with non-acute VTE undergoing autologous stem cell transplantation may offer the best risk-benefit tradeoff17.
Mitigating the bleeding risk
The 50×109/L platelet transfusion threshold recommended with therapeutic anticoagulation in acute settings11,12 is based on expert opinion5 and its effect on outcomes is unclear17. This strategy has implications on blood bank resources and is associated with high rates of transfusion-related adverse events19 and early AC discontinuation16,17,19. Taken together, increased platelet transfusion threshold is not without risk, while the ideal threshold and effect thereof is not clear. Reduction in anticoagulation doses is an integral part of guidelines11-13 mostly supported by low grade evidence from other thrombocytopenic settings showing low bleeding risks with sub-optimal doses of LMWH or heparin15,21-26. However, data on outcomes with reduced vs. full doses for VTE in thrombocytopenia are sparse and conflicting14,15,20. Taken together, there may be a relatively low bleeding risk with prophylactic doses in these patients but the safety regarding recurrent thrombosis remains unclear.
Knowledge gaps
Some of the main content gaps are data on non-acute VTE, non-LMWH anticoagulation, non-VTE anticoagulation indications (e.g. atrial fibrillation) and the effect of platelet transfusion thresholds on bleeding. Moreover, there is no data on management of antiplatelet medication in thrombocytopenia, outside the setting of aspirin in acute myocardial infarction (MI)27. A few of these gaps are being addressed by ongoing studies28-30.
Summary and recommendations
For settings in which no guidelines exist, such as non-VTE indications for anticoagulation, the recommendations for use of LMWH in VTE can be adapted while considering differences in risk-benefit ratios and especially thrombotic risk. Aspirin use in acute MI in thrombocytopenic patients (especially >30 x 109/L) should be strongly considered and discussed on a case-by-case basis27. In addition, consider the following general recommendations:
- Always reevaluate the indication for chronic antithrombotic therapy;
- Formulate a clear management plan, to be reassessed frequently;
- Consider returning to full anticoagulation doses after platelet count recovers (>50 x 109/L), even between treatment cycles, if the indication remains16;
- When using the guidelines remember that the supporting evidence is weak. Accordingly, deviations may be contemplated for specific patients, while considering the evidence presented in this review.
References
- Donnellan E, Khorana AA. Cancer and Venous Thromboembolic Disease: A Review. Oncologist. 2017;22(2):199-207.
- Liebman HA. Thrombocytopenia in cancer patients. Thromb Res. 2014;133 Suppl 2:63.
- Leader A, ten Cate V, ten Cate-Hoek A, et al. Anticoagulation in Thrombocytopenic Patients with Hematological Malignancy: A Multi-center, Multinational Decision Making Analysis. 9th ICTHIC congress, Bergamo, Italy, April 13-15, 2018, Abstract no. 1152; April 13-15 2018; .
- Vinholt PJ, Alnor A, Nybo M, Hvas A. Prediction of bleeding and prophylactic platelet transfusions in cancer patients with thrombocytopenia. Platelets. 2016;27(6):547-554.
- Saccullo G, Marietta M, Carpenedo M, et al. Platelet Cut-Off For Anticoagulant Therapy In Cancer Patients With Venous Thromboembolism and Thrombocytopenia: An Expert Opinion Based On RAND/UCLA Appropriateness Method (RAM). Blood. 2013;122(21):581.
- Ibrahim RB, Skewes MD, Kuriakose P. ‘Sailing in troubled waters’: a review of the use of anticoagulation in adult cancer patients with thrombocytopenia. Blood Coagul Fibrinolysis. 2016;27(6):615-630.
- Lee AYY, Levine MN, Baker RI, et al. Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med. 2003;349(2):146-153.
- Lee AYY, Kamphuisen PW, Meyer G, et al. Tinzaparin vs Warfarin for Treatment of Acute Venous Thromboembolism in Patients With Active Cancer: A Randomized Clinical Trial. JAMA. 2015;314(7):677-686.
- Raskob GE, van Es N, Verhamme P, et al. Edoxaban for the Treatment of Cancer-Associated Venous Thromboembolism. N Engl J Med. 2017;.
- Schiffer CA, Bohlke K, Delaney M, et al. Platelet Transfusion for Patients With Cancer: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol. 2018;36(3):283-299.
- Carrier M, Khorana AA, Zwicker JI, Noble S, Lee AYY. Management of challenging cases of patients with cancer-associated thrombosis including recurrent thrombosis and bleeding: guidance from the SSC of the ISTH. J Thromb Haemost. 2013;11(9):1760-1765.
- Easaw JC, Shea-Budgell MA, Wu CMJ, et al. Canadian consensus recommendations on the management of venous thromboembolism in patients with cancer. Part 2: treatment. Curr Oncol. 2015;22(2):144-155.
- Cancer-Associated Venous Thromboembolic Disease (Version 1.2017) [Internet]. [cited February 7, 2018].
- Kopolovic I, Lee AYY, Wu C. Management and outcomes of cancer-associated venous thromboembolism in patients with concomitant thrombocytopenia: a retrospective cohort study. Ann Hematol. 2015;94(2):329-336.
- Khanal N, Bociek RG, Chen B, et al. Venous thromboembolism in patients with hematologic malignancy and thrombocytopenia. Am J Hematol. 2016;91(11):E472.
- Houghton DE, Key NS, Zakai NA, Laux JP, Shea TC, Moll S. Analysis of anticoagulation strategies for venous thromboembolism during severe thrombocytopenia in patients with hematologic malignancies: a retrospective cohort. Leuk Lymphoma. 2017;58(11):2573-2581.
- Li A, Davis C, Wu Q, et al. Management of venous thromboembolism during thrombocytopenia after autologous hematopoietic cell transplantation. Blood Adv. 2017;1(12):707-714.
- Mantha S, Miao Y, Wills J, Parameswaran R, Soff GA. Enoxaparin dose reduction for thrombocytopenia in patients with cancer: a quality assessment study. J Thromb Thrombolysis. 2017;43(4):514-518.
- Samuelson Bannow BT, Walter RB, Gernsheimer TB, Garcia DA. Patients treated for acute VTE during periods of treatment-related thrombocytopenia have high rates of recurrent thrombosis and transfusion-related adverse outcomes. J Thromb Thrombolysis. 2017;44(4):442-447.
- Pemmaraju N, Kroll MH, Afshar-Kharghan V, Oo TH. Bleeding Risk in Thrombocytopenic Cancer Patients with Venous Thromboembolism (VTE) Receiving Anticoagulation. Blood. 2012;120(21):3408.
- Or R, Nagler A, Shpilberg O, et al. Low molecular weight heparin for the prevention of veno-occlusive disease of the liver in bone marrow transplantation patients. Transplantation. 1996;61(7):1067-1071.
- Simon M, Hahn T, Ford LA, et al. Retrospective multivariate analysis of hepatic veno-occlusive disease after blood or marrow transplantation: possible beneficial use of low molecular weight heparin. Bone Marrow Transplant. 2001;27(6):627-633.
- Herishanu Y, Misgav M, Kirgner I, Ben-Tal O, Eldor A, Naparstek E. Enoxaparin can be used safely in patients with severe thrombocytopenia due to intensive chemotherapy regimens. Leuk Lymphoma. 2004;45(7):1407-1411.
- Monreal M, Zacharski L, Jiménez JA, Roncales J, Vilaseca B. Fixed-dose low-molecular-weight heparin for secondary prevention of venous thromboembolism in patients with disseminated cancer: a prospective cohort study. J Thromb Haemost. 2004;2(8):1311-1315.
- Ibrahim RB, Peres E, Dansey R, et al. Safety of low-dose low-molecular-weight-heparins in thrombocytopenic stem cell transplantation patients: a case series and review of the literature. Bone Marrow Transplant. 2005;35(11):1071-1077.
- Saccullo G, Malato A, Raso S, et al. Cancer patients requiring interruption of long-term warfarin because of surgery or chemotherapy induced thrombocytopenia: the use of fixed sub-therapeutic doses of low-molecular weight heparin. Am J Hematol. 2012;87(4):388-391.
- Feher A, Kampaktsis PN, Parameswaran R, Stein EM, Steingart R, Gupta D. Aspirin Is Associated with Improved Survival in Severely Thrombocytopenic Cancer Patients with Acute Myocardial Infarction. Oncologist. 2017;22(2):213-221.
- Management and Outcomes of Anti-thrombotic Medication Use in Thrombocytopenia – Full Text View – ClinicalTrials.gov [Internet]. [cited Jan 25, 2018]. Available from: https://clinicaltrials.gov/ct2/show/NCT03288441.
- Thromboprophylaxis of Venous Thromboembolism in Acutely-ill Medical Inpatients With Thrombocytopenia – Full Text View – ClinicalTrials.gov [Internet]. [cited Jan 25, 2018]. Available from: https://clinicaltrials.gov/ct2/show/NCT01727401.
- Management of Platelet Transfusion Therapy in Patients With Blood Cancer or Treatment-Induced Thrombocytopenia – Full Text View – ClinicalTrials.gov [Internet]. [cited Jan 25, 2018]. Available from: https://clinicaltrials.gov/ct2/show/NCT03195010.
