There is ample evidence confirming that cancer predisposes to thrombosis, while products of activation of the coagulation system, e.g., tissue factor and thrombin, precipitate tumor growth. Affected women frequently present with specific types of cancer related to reproductive organs, such as breast, uterus and ovary. These organs are strongly influenced by hormones, especially estrogen, and part of the treatment in these cases is directed to blocking the hormonal stimulus. Drugs interfering with the hormonal cycle, including tamoxifen, a partial estrogen receptor antagonist, and aromatase inhibitors, a class of drugs inhibiting estrogen synthesis, have been demonstrated to increase the risk of thrombosis by 2- and 1.6-fold, respectively. As these drugs are given for several years to prevent breast cancer recurrence, the issue of prophylactic anticoagulant therapy duration in women with a prior thrombotic event requires further investigation. Several reports also point to an increased risk of thrombosis associated with the application of other measures to block the sex hormone production, such as luteinizing hormone-releasing hormone (LHRH) analogs and Megestrol acetate (Megace), a progesterone derivative drug. Thus, the use of these preparations in patients with other significant thrombotic risk factors should be carefully considered. In women with any active cancer, combined hormonal contraceptives are not recommended due to an increased risk of thrombosis. Progesterone-only preparations, taken either orally or as an intrauterine device, are probably safe in terms of thrombotic risk.
The use of sex hormones as oral contraceptives or hormonal replacement therapy (HRT), especially those comprising estrogen, is established to be associated with an elevated risk of thrombosis. In addition, estrogen is known to contribute to tumor growth and induction of intracellular signaling mainly occurs via the estrogen receptor. The effects of hormones on tumor growth are not restricted to tumors developing in reproductive organs only. Estrogen has also been found to enhance tumor cell proliferation and angiogenesis in non-hormonal dependent tumors, such as lymphoma, meduloblastoma and germ-cell tumor. Along the same lines, , large observational studies have reported that estrogen-progestin therapy appears to increase the risk of breast cancer, ovarian cancer and endometrial cancer.
Breast and cervix cancers account for about 50% of pregnancy-related malignancies, followed by lymphoma and leukemia. The diagnosis of cancer during pregnancy poses a major burden on the woman and her family. With an estimated prevalence of one per thousand pregnancies, cancer is considered to be the second leading cause of maternal mortality after pregnancy-associated vascular complications. The hypercoagulability state in pregnant women with cancer may lead to placental thrombosis, fetal growth restriction or loss, and venous thromboembolism (VTE).
The mechanism of cancer and thrombosis
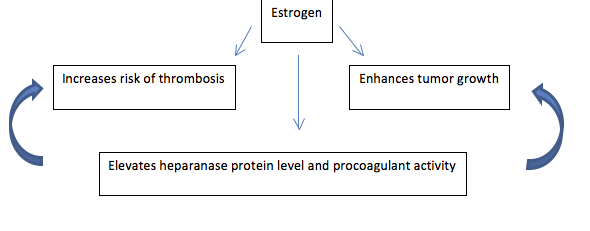 Heparanase protein, which is known to be involved in angiogenesis and metastasis, has been shown to affect the hemostatic system. It forms a complex with tissue factor (TF) and enhances the generation of activated factor X (FXa), thus contributing to activation of the coagulation system. Estrogen has been demonstrated to upregulate the expression of heparanase, resulting in increased tumor growth along with intensified activation of the hemostatic system. Hence, heparanase may affect tumor growth and augment the risk of thrombosis. Elevated heparanase levels and procoagulant activity have been observed in women using oral contraceptives, women at the end of pregnancy, in placentas obtained in early pregnancy losses and in patients with lung cancer. An assay measuring heparanase procoagulant activity could potentially evaluate the combined effect of cancer and estrogen on the increased risk of thrombosis.
Heparanase protein, which is known to be involved in angiogenesis and metastasis, has been shown to affect the hemostatic system. It forms a complex with tissue factor (TF) and enhances the generation of activated factor X (FXa), thus contributing to activation of the coagulation system. Estrogen has been demonstrated to upregulate the expression of heparanase, resulting in increased tumor growth along with intensified activation of the hemostatic system. Hence, heparanase may affect tumor growth and augment the risk of thrombosis. Elevated heparanase levels and procoagulant activity have been observed in women using oral contraceptives, women at the end of pregnancy, in placentas obtained in early pregnancy losses and in patients with lung cancer. An assay measuring heparanase procoagulant activity could potentially evaluate the combined effect of cancer and estrogen on the increased risk of thrombosis.
Cancer involving reproductive organs has a significant psychological bearing on the woman’s self-image, given an inevitable impact on the life of her children and family, a potential effect on the ability to carry more children and the associated concern about her own future. In addition, blocking the hormonal effect leading to the cessation of the menstrual cycle may result in mood disturbances and accelerated osteoporosis. Specific risk scoring systems and guidelines aiming to prevent thrombosis related to the use of drugs interfering with the hormonal cycle should be developed to ameliorate the above conditions.
